By Ray Peat – 50+ Years of Fraud
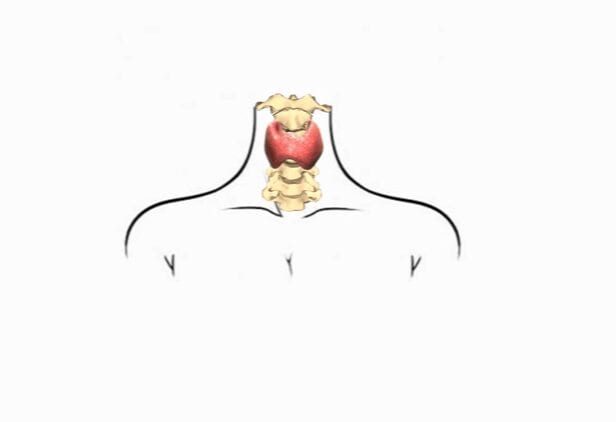
Until the second world war, hypothyroidism was diagnosed on the basis of BMR (basal metabolic rate) and a large group of signs and symptoms. In the late 1940s, promotion of the (biologically inappropriate) PBI (protein-bound iodine) blood test in the U.S. led to the concept that only 5% of the population were hypothyroid, and that the 40% identified by “obsolete” methods were either normal, or suffered from other problems such as sloth and gluttony, or “genetic susceptibility” to disease. During the same period, thyroxine became available, and in healthy young men it acted “like the thyroid hormone.” Older practitioners recognized that it was not metabolically the same as the traditional thyroid substance, especially for women and seriously hypothyroid patients, but marketing, and its influence on medical education, led to the false idea that the standard Armour thyroid USP wasn’t properly standardized, and that certain thyroxine products were; despite the fact that both of these were shown to be false.
By the 1960s, the PBI test was proven to be irrelevant to the diagnosis of hypothyroidism, but the doctrine of 5% hypothyroidism in the populaton became the basis for establishing the norms for biologically meaningful tests when they were introduced.
Meanwhile, the practice of measuring serum iodine, and equating it with “thyroxine the thyroid hormone,” led to the practice of examining only the iodine content of the putative glandular material that was offered for sale as thyroid USP. This led to the substitution of materials such as iodinated casein for desiccated thyroid in the products sold as thyroid USP. The US FDA refused to take action, because they held that a material’s iodine content was enough to identify it as “thyroid USP.” In this culture of misunderstanding and misrepresentation, the mistaken idea of hypothyroidism’s low incidence in the population led to the acceptance of dangerously high TSH (thyroid stimulating hormone) activity as “normal.” Just as excessive FSH (follicle stimulating hormone) has been shown to have a role in ovarian cancer, excessive stimulation by TSH produces disorganization in the thyroid gland.
Tests & the “free hormone hypothesis”
After radioactive iodine became available, many physicians would administer a dose, and then scan the body with a Geiger counter, to see if it was being concentrated in the thyroid gland. If a person had been eating iodine-rich food (and iodine was used in bread as a preservative/dough condition, and was present in other foods as an accidental contaminant), they would already be over saturated with iodine, and the gland would fail to concentrate the iodine. The test can find some types of metastatic thyroid cancer, but the test generally wasn’t used for that purpose. Another expensive and entertaining test has been the thyrotropin release hormone (TRH) test, to see if the pituitary responds to it by increasing TSH production. A recent study concluded that “TRH test gives many misleading results and has an elevated cost/benefit ratio as compared with the characteristic combination of low thyroxinemia and non-elevated TSH.” (Bakiri, Ann. Endocr (Paris) 1999), but the technological drama, cost, and danger (Dokmetas, et al., J Endocrinol Invest 1999 Oct; 22(9): 698-700) of this test is going to make it stay popular for a long time. If the special value of the test is to diagnose a pituitary abnormality, it seems intuitively obvious that overstimulating the pituitary might not be a good idea (e.g., it could cause a tumor to grow).
Everything else being equal, as they say, looking at the amount of thyroxine and TSH in the blood can be informative. The problem is that it’s just a matter of faith that “everything else” is going to be equal. The exceptions to the “rule” regarding normal ranges for thyroxine and TSH have formed the basis for some theories about “the genetics of thyroid resistance,” but others have pointed out that, when a few other things are taken into account, abnormal numbers for T4, T3, TSH, can be variously explained.
The actual quantity of T3, the active thyroid hormone, in the blood can be measured with reasonable accuracy (using radioimmunoassay, RIA), and this single test corresponds better to the metabolic rate and other meaningful biological responses than other standard tests do. But still, this is only a statistical correspondence, and it doesn’t indicate that any particular number is right for a particular individual.
Therapy
Years ago it was reported that Armour thyroid, U.S.P., released T3 and T4, when digested, in a ratio of 1:3, and that people who used it had much higher ratios of T3 to T4 in their serum, than people who took only thyroxine. The argument was made that thyroxine was superior to thyroid U.S.P., without explaining the significance of the fact that healthy people who weren’t taking any thyroid supplement had higher T3:T4 ratios than the people who took thyroxine, or that our own thyroid gland releases a high ratio of T3 to T4. The fact that the T3 is being used faster than T4, removing it from the blood more quickly than it enters from the thyroid gland itself, hasn’t been discussed in the journals, possibly because it would support the view that a natural glandular balance was more appropriate to supplement than pure thyroxine.
Glandulars
-
Sale!

Thyroid 100 Vegicaps 40 mg
Original price was: $34.99.$29.99Current price is: $29.99. -

-

-

Hypothalamus 100 Vegicaps
$99.64 -

Kidney Beef 100 vcaps
$20.87 -

-

Beef Heart 180 caps
$42.99 -

Liver Beef 1000mg 125 vcaps
$26.85 -
Liver Powder Beef 200 grams
$26.85 -

Pancreas Pork 60/720 Vegicaps 425 mg
$26.89 – $198.94 -

Thymus 1000mg 75 Vcaps
$37.98 -






























![WHO issues warning about the next potential pandemic [H5N1] 987051f7316da70abd81be391e8261f9 863287870 WHO issues warning about the next potential pandemic [H5N1]](https://www.holistichealthonline.info/wp-content/uploads/2023/02/987051f7316da70abd81be391e8261f9-863287870.jpg)